WHAT IS A CCBHC?
The Excellence in Mental Health Act demonstration established a federal definition and criteria for Certified Community Behavioral Health Clinics (CCBHCs).
For more information, please visit the National Council’s CCBHC Resource Hub or contact Rebecca David at (202) 684-3735 or RebeccaD@TheNationalCouncil.org.
These entities, a new provider type in Medicaid, are designed to provide a comprehensive range of mental health and substance use disorder services to vulnerable individuals. In return, CCBHCs receive an enhanced Medicaid reimbursement rate based on their anticipated costs of expanding services to meet the needs of these complex populations.
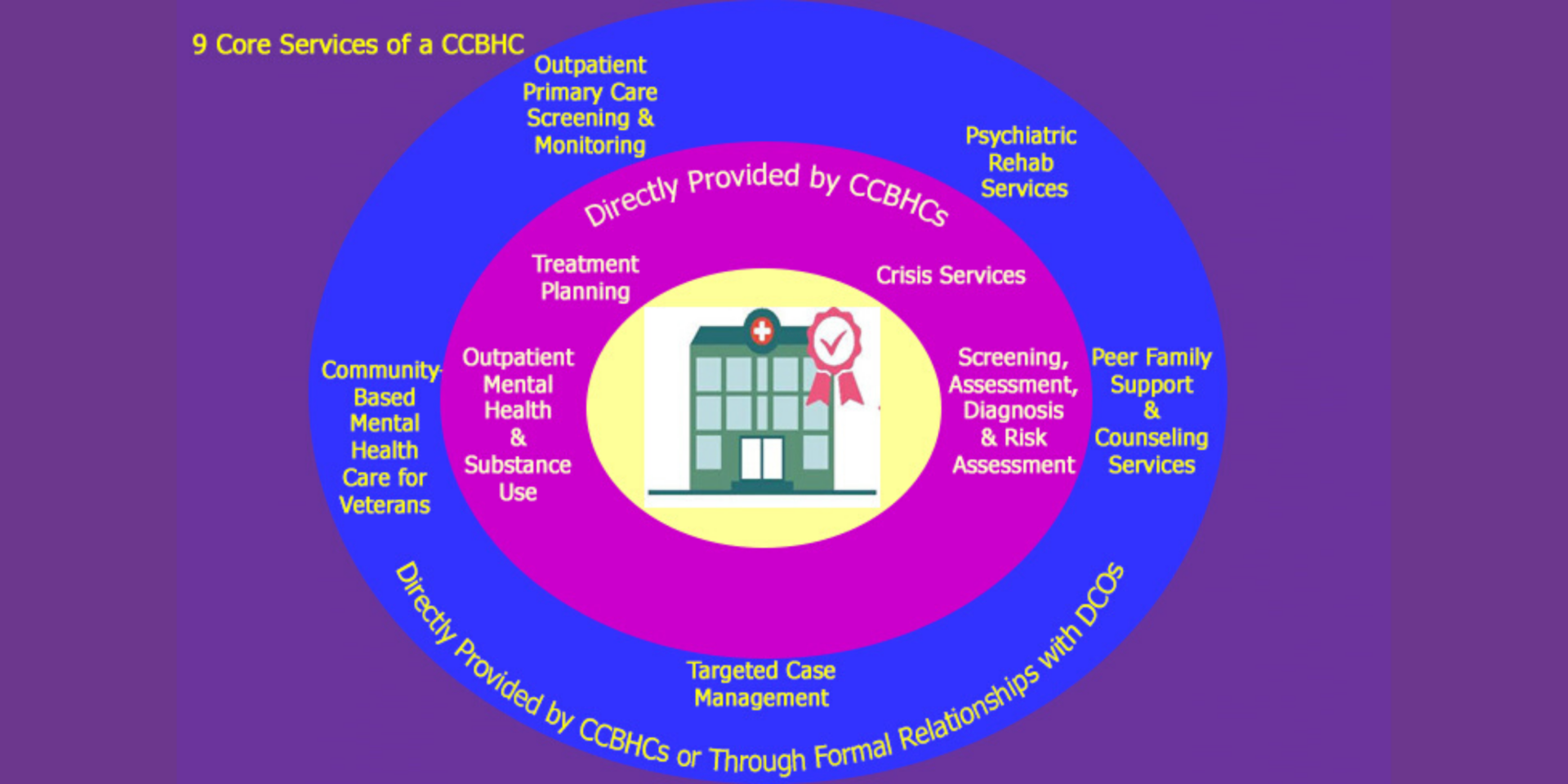
CCBHCs are responsible for directly providing (or contracting with partner organizations to provide) nine types of services, with an emphasis on the provision of 24-hour crisis care, utilization of evidence-based practices, care coordination and integration with physical health care. The demonstration program represents the largest investment in mental health and addiction care in generations.
COMPREHENSIVE CARE IS KEY
- 24/7/365 crisis services to help people stabilize in the most clinically appropriate, least restrictive, least traumatizing, and most cost-effective settings.
- Immediate screening and risk assessment for mental health, addictions and basic primary care needs to ameliorate the chronic co-morbidities that drive poor health outcomes and high costs for those with behavioral health disorders.
- Easy access to care with criteria to assure a reduced wait time so those who need services can receive them when they need them, regardless of ability to pay or location of residence.
- Tailored care for active duty military and veterans to ensure they receive the unique health support essential to their treatment.
*May be provided directly by CCBHC or through contract with Designated Collaborating Organization
CCBHCs must provide crisis mental health services; screening, assessment and diagnosis; patient-centered treatment planning; outpatient mental health and substance use services; primary care screening and monitoring;* targeted case management;* psychiatric rehabilitation services:* peer support, counseling and family support services; and services for veterans.*
- Expanded care coordination with other health care providers, social service providers and law enforcement, with a focus on whole health and comprehensive access to a full range of medical, behavioral and supportive services.
- Commitment to peers and family, recognizing that their involvement is essential for recovery and should be fully integrated into care.
*May be provided directly by CCBHC or through contract with Designated Collaborating Organization
WHO IS SERVED BY CCBHCS?
CCBHCs are available to any individual in need of care, including, but not limited to, people with serious mental illness, serious emotional disturbance, long-term chronic addiction, mild or moderate mental illness and substance use disorders and complex health profiles.
CCBHCs will provide care regardless of ability to pay, caring for those who are underserved; have low incomes; are insured, uninsured or on Medicaid; and those who are active duty military or veterans.
ADDRESSING FINANCING BARRIERS
Financing has emerged as a critical issue in increasing Americans’ access to behavioral health services. CCBHCs were specifically designed to address financing shortfalls by paying clinics a Medicaid rate that is inclusive of their anticipated costs of expanding their service lines and serving new consumers. Through a prospective payment system that is similar to one already in place for other safety-net providers, the Excellence Act supports:
- Expanded access to care through an enhanced workforce. CCBHCs’ Medicaid rates cover costs associated with hiring new staff, such as licensed counselors or peer support specialists, paying employees a competitive wage in the local market and training staff in required competencies, such as care coordination and evidence-based practices.
- A stronger response to the addiction crisis. Addiction care is embedded throughout the CCBHC range of services, including screening for substance use disorders, detoxification, outpatient addiction services, peer support services and other addiction recovery services at state discretion. Importantly, most states participating in the CCBHC program have also made medication-assisted treatment (MAT) a required service.
- Enhanced patient outreach, education, and engagement. CCBHCs’ Medicaid rates include the cost of activities that have traditionally been nearly impossible to reimburse yet play a critical role in behavioral health services.
- Care where people live, work and play. CCBHCs may receive Medicaid payment for services provided outside the four walls of their clinic: for example, via mobile crisis teams, home visits, outreach workers and emergency or jail diversion programs.
- Electronic exchange of health information for care coordination purposes. CCBHCs’ Medicaid rates include the cost of purchasing or upgrading electronic systems to support electronic information exchange.
- The Excellence Act prioritizes improving the adoption of technological innovations for care, including data collection, quality reporting and other activities that bolster providers’ ability to care for individuals with co-occurring disorders.
